Tuberculosis: Disparities in Indigenous populations
Tuberculosis appears on the list of the world’s top 10 causes of death. Although the global incidence of tuberculosis is decreasing by 2% per year, this disease is still common in some Indigenous populations.
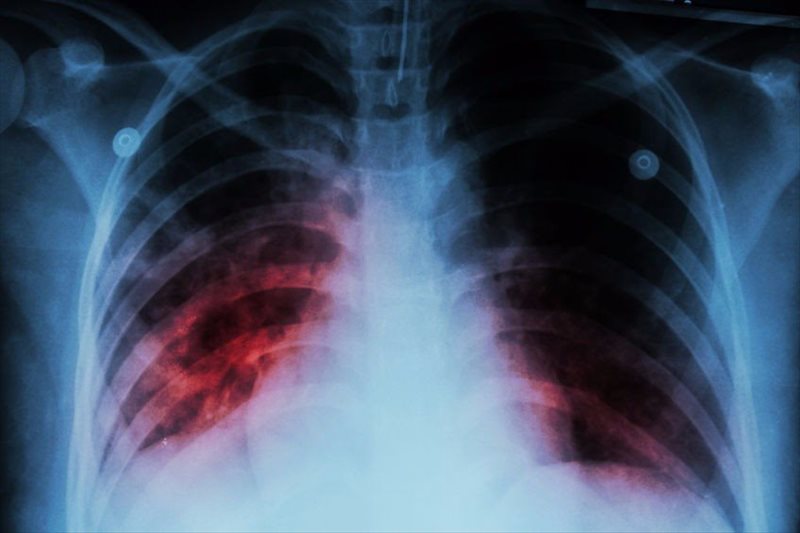
Tuberculosis is a bacterial infection that generally affects the lungs. Individuals can be infected with tuberculosis but show no signs of disease, a situation termed latent tuberculosis. Symptoms of tuberculosis are more likely to manifest in those who are in poor health or from low socioeconomic backgrounds – those who are least able to afford the healthcare costs associated with this disease.
The incidence of tuberculosis is higher in Indigenous populations
Tuberculosis has greatly impacted Indigenous populations throughout North America and Greenland. In the 1950s, notification rates ranged from 1500-2500 per 100,000 individuals. The advent of population-based intervention trials saw the annual notification rates drop by 15-20%. Yet, notification rates began to increase in the late 1980s in some Indigenous populations.
There is, therefore, some debate as to whether the original decline in notification rates was due to effective intervention strategies, or if overall improvements in health and socioeconomic backgrounds contributed to this, or both.
A Canadian team investigated this issue in six Indigenous populations: First Nations in Alberta, Alaska Native population, Cree population of Eeyou Istchee or Cree Territory of James Bay in Quebec, and the Inuits of Nunavut, the Inuits of Nunavik in North Quebec, and the Inuits of Greenland.
The team looked at 54-years worth of tuberculosis notification rates (1960-2014) for the six populations. They then examined whether three intervention strategies—the bacillus Calmette-Guerin (BCG) vaccination given to infants, chest radiography screening for active symptoms of tuberculosis, and latent tuberculosis testing and treatment—influenced these rates.

Intervention decreases the incidence of tuberculosis
The team’s findings, published in Lancet Public Health, showed that the incidence of tuberculosis decreased dramatically from 310-536 cases per 100,000 individuals to 62-90 per 100,000 in all six populations between 1960 and 1980.
Although several health and socioeconomic factors were considered, the team believe that this decrease was attributed to two of the three interventions – the BCG vaccination decreased the tuberculosis incidence by 11%, and latent tuberculosis testing and treatment decreased it by 10%. These interventions also helped to increase the overall life expectancy and decrease infant mortality in these populations.
A disparity in the incidence of tuberculosis
This trend continued in three Indigenous populations – the First Nations, Alaska Native, and Cree populations – with the incidence of tuberculosis plummeting to 18 per 100,000 individuals in 2014. This mirrored the trend observed in the general Canadian population, although the numbers were much lower. Yet, despite overall improvements in general health and socioeconomic factors for all six populations during this time period, there was a resurgence of tuberculosis in the three Inuit populations, with the incidence increasing to 157 per 100,000 individuals by 2014.
The team believe that significant disparities between the six Indigenous populations contributed to this finding. The three populations in which tuberculosis continually decreased were less likely to be smokers, had higher education levels and were more likely to have diabetes and obesity.
Tuberculosis interventions discontinued prematurely
The intervention strategies were readily accepted by a large proportion of the Indigenous populations, hence the rapid decrease in notification rates. It is likely that these interventions were discontinued based on the successful decrease in notification rates, although there were no records behind these decisions. The authors speculate that the resurgence of tuberculosis in the Inuit populations may be associated with the premature discontinuation of these programs.
Effective and Acceptable Programs are required
This study was subject to inconsistencies in data collection and diagnosis of tuberculosis over the 54-year period. Despite these limitations, the team clearly demonstrated that intervention strategies to prevent tuberculosis worked in the six Indigenous populations studied. However, the resurgence of tuberculosis in a subset of these populations indicates that longer-running intervention strategies must be re-implemented. These must be cost efficient, effective, and readily accepted by the target population if they are to contribute to the World Health Organization’s aim to eliminate tuberculosis by 2035.
Written by Natasha Tetlow, PhD
References:
- Dehghani K, et al. Determinants of tuberculosis trends in six Indigenous populations of the USA, Canada, and Greenland from 1960 to 2014: a population-based study. Lancet Public Health. 2018. 3: e0133-42. http://dx.doi.org/10.1016/ S2468-2667(18)30002-1.
- World Health Organization. Tuberculosis Fact Sheet. Published 16 February 2018. Available at: www.who.int/news-room/fact-sheets/detail/tuberculosis
Need to get in touch?
Address: 8054 Yonge Street Thornhill, Ontario L4J 1W3
Phone: (905) 886 1212
Latest articles
April 28, 2024
April 28, 2024
April 28, 2024
April 28, 2024
April 28, 2024