Covered by OHIP?
Most services are covered by the Ontario Health Insurance Plan (OHIP)
Waiting Time
Your timeframe depends on the type of procedure.
OHIP Covered Services
Most services are covered by the Ontario Health Insurance Plan (OHIP)
WILDERMAN MEDICAL CLINIC
What is pudendal neuralgia?
Pudendal neuralgia (PN), which may also be called pudendal nerve entrapment syndrome, is a chronic pain condition caused by unilateral (<50% of cases) or bilateral (>50% of cases) irritation or damage to the pudendal nerve (Leslie, 2022).
This pain worsens when you are sitting and gets better while standing or lying down. It is often the result of trauma to the pelvis, whether in the form of repeated injuries or a sudden major one, that causes the nerve to become damaged in some way.
There are four distinct types of Pudendal Neuralgia:
• Type 1: The nerve is damaged/irritated as it leaves the tailbone (coccyx) and passes by the piriform muscle.
• Type 2: The nerve is affected between the tailbone (coccyx) and anus as it is caught between two ligaments (this is the most common type of PN).
• Type 3: The nerve is damaged/irritated between the anus and genitals as it passes through the Alcock’s canal.
• Type 4: The nerve is affected at or after it separates into the terminal branches around the genitals.
As PN is a relatively new diagnosis to designate a specific kind of chronic pelvic or genital pain, there is no consistent estimate of how many people are affected. It is estimated to account for 4% of all chronic pelvic pain diagnoses, though the percentage is likely to be much higher than that.
Similarly, the lack of consistent diagnosis means that research on PN is ongoing, and most of the current knowledge is based on gathered medical professional experience rather than research.
Anatomy of the perineum and pudendal nerve
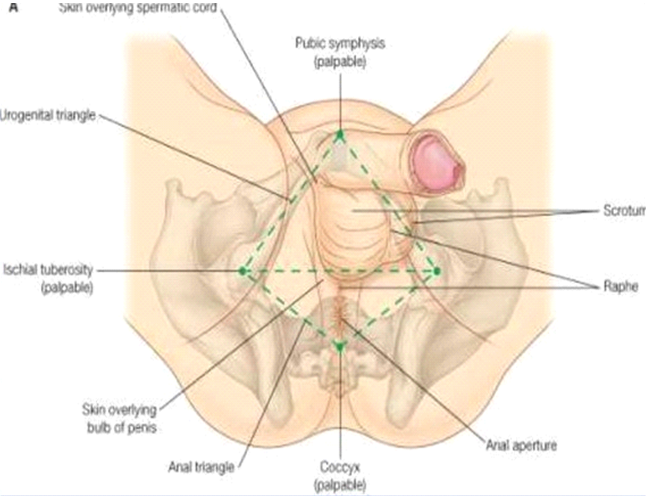
The perineum is a diamond-shaped area that starts at your tailbone (coccyx) and ends just above the genitalia (Grujičić, 2022). Its sides reach from one thigh to the other.
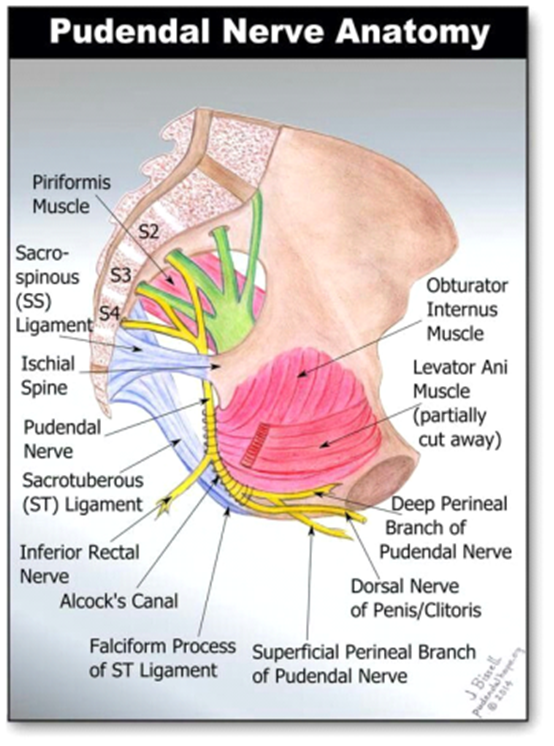
The pudendal nerve is responsible for motor control and sensory information of the perineum and genitalia. It divides itself into four branches that extend throughout the perineum, all of which can be involved in PN.
This nerve is involved in the sexual stimulation of the genitals as well as urination and defecation, and damage to the pudendal nerve can adversely affect these functions.
Risk factors for pudendal neuralgia
The current results of research and medical professionals’ experiences have highlighted several possible factors that increase the risk of PN (Leslie et al., 2022). These include:
• Size of the pelvis: A wide pelvis increases the risk of pinching or irritating the nerve as it may be closer to the surrounding tissues than in thinner pelvises. As such, there is an estimated 7 women (AFAB) for every 3 men (AMAB) affected by PN.
• Activities that put repeated pressure on the tailbone (coccyx): As PN is a chronic irritation of the pudendal nerve, any repeated activities that involve pressure on the tailbone (coccyx) region will increase the risk of PN. These activities include repeated squats, consistent cycling over rough terrain, horseback riding, and rowing.
• Prolonged and chronic sitting: Sitting puts pressure on the tailbone (coccyx); as such, people who spend large amounts of time sitting in a single position have a higher risk of developing PN.
• Pelvic area surgeries: All surgeries may cause some level of inflammation, though often minor and temporary. Pelvic surgery may put increased pressure on the pudendal nerve, due to inflammation or the method of surgery itself, which may cause PN.
• Chronic urinary issues and/or constipation: As the pudendal nerve is involved in urination and defecation, chronic straining during those activities may lead to damage or irritation to the nerve.
Causes
In addition to the risk factors listed above, some other common causes of pudendal neuralgia include:
• Pelvic trauma
• Radiation therapy for cancers in the pelvic region
• Prolonged and/or traumatic childbirth
• Repeated activities that put pressure on the hip joints and/or use your pelvic muscles
• Viral infections, including chronic urinary tract and/or vaginal infection, herpes, HIV
Some uncommon causes of PN include diabetes, multiple sclerosis, benign tumors, and/or lesions on the pudendal nerve.
Symptoms of Pudendal Neuralgia
Common symptoms of PN include:
• Chronic pain that worsens when sitting down and improves when standing or lying down
• Chronic pain that worsens as the day progresses
• Increased sensitivity to touch, often painful, in the lower pelvic area
• Painful urination or defecation
• Increased need to urinate
• New pain during sexual activities
• Erectile dysfunction
• Difficulty reaching orgasms
• Swollen anus or perineum
Most PN patients have described the pain as a burning sensation, with occasional stabbing or aching sensations.
If the nerve damage becomes severe, the pain may transform into numbness and/or a loss of feeling in the affected areas. This numbness has been described as pins-and-needles shocks.
How does pudendal neuralgia develop?
The progression of PN tends to be linear. It often starts with bladder issues, causing minor pain or discomfort.
As the damage or irritation to the nerve increases, the pain will also increase and spread to other areas. The specific areas affected and the type of symptoms will depend on the type of PN.
How is pudendal neuralgia diagnosed?
In 2008, Labat et al. created a set of criteria, called the Nantes Criteria, to diagnose PN more effectively. This new tool sets out a set series of symptoms and tests to be used by medical professionals to identify patients with PN. An outline of these diagnostic criteria can be found at:
https://www.orpha.net/data/patho/Pro/en/Pudendal_Diag_criteria_EN.pdf
Additionally, your doctor will ask you if you have had a recent pelvic injury, what kind of exercises you do and how often, and your past medical history. They may test your reflexes and senses in the affected areas.
If your doctor is unsure if you have PN, they may recommend an MRI to rule out any other causes of your symptoms.
How is pudendal neuralgia treated?
The treatment of PN borrows a lot from the common approaches to treating chronic pain disorders. As PN can be caused by damage to the nerve and is often diagnosed after years of pain and symptoms, the current treatment for PN aims to reduce and manage your symptoms.
The common and recent consensus on the approach to treating PN is divided into two levels of treatment: non-invasive and invasive (Levesque et al., 2022), also referred to as non-interventional and interventional treatments.
The non-invasive treatments should be attempted first under the supervision of medical professionals before considering more invasive treatments.
Non-invasive treatments for pudendal neuralgia include:
• Physiotherapy: The goal of PN physiotherapy may depend on the severity and underlying cause of your symptoms. The exercises will focus on strengthening the pelvic floor muscles and relaxing any strained muscles. The recommended length for PN physiotherapy is between 6-12 weeks though it may be changed to accommodate the needs of the patients.
• Behavior changes: To reduce any chronic pressure that leads to PN, it is suggested that changes are made to a patient’s behavior such as reducing strenuous activities and/or breaking up time seated with periods of standing or lying down.
• Environmental changes: Seeing an occupational therapist in order to change the work and/or home environment to reduce possible sources of pressure on the tailbone/coccyx. Common suggestions are buying a donut pillow to add to any seats, getting a standing desk, and improving the cushions of seats.
• Medications: As PN can be caused by viral infections, antiviral treatment may be advised. The use of non-steroidal anti-inflammatory medications (NSAIDs) to address inflammation, and the use of muscle relaxants may be needed as well. Other medications to help manage pain may be recommended if physiotherapy and other medications do not provide sufficient pain relief. A review of research on the treatment of nerve pain suggests that anti-epileptic medication may provide better and safer pain relief compared to narcotics (Finnerup et al., 2015).
• Psychological treatment: Chronic pain is frequently associated with mental health issues such as anxiety and depression. As such, patients with PN are encouraged to seek professional mental health support. This may include the use of anti-anxiety and antidepressant medications, as well as psychotherapy.
• Transcutaneous electrical nerve stimulation (TENS): While there is no specific research linking the use of TENS as a treatment for PN, there is sufficient research showing its effective and safe use to reduce nerve-related pain for experts to recommend its use for PN.
If these non-invasive treatments do not provide enough pain relief for the patient, the following treatments may be considered:
• Pudendal nerve block injections: This treatment should only be considered if the patient responds positively to the diagnostic injections with a reduction of pain > 50% for at least 3 weeks (Wang et al., 2022). Patients whose PN started > 4 years ago, who have a complete loss of feeling in the affected areas, and with Type 4 PN should not be considered for this treatment.
• High-voltage long-duration pulsed radiofrequency: Pulsed radiofrequency is used to treat nerve pain by reducing the nerve’s ability to transmit pain signals. However, the typical treatment does not provide consistent relief for PN. Wang & Song (2021) found that PN responded significantly to a modified treatment. This modified treatment was obtained by increasing the duration and intensity of pulsed radiofrequency treatments. Their research showed 88% of patients reported significant pain relief at a 12-week follow-up.
• Decompression surgery: This surgery is considered to be the treatment that offers the most consistent and long-lasting relief of PN symptoms. The surgery opens up the area around the nerve to reduce the pressure on it, and then a protective mesh is installed to prevent any further damage or irritation to the nerve.
• Neuromodular implants: This surgery installs an implant on the pudendal nerve that limits the intensity of signals that pass through it. This should only be considered if no other treatments have provided any effective relief.
However, due to the limited research specifically done about PN, further studies are needed to determine the optimal treatment plan for PN. Most of the current suggested treatments are based on research regarding chronic pelvic pain and chronic nerve pain conditions.
What do we do at WMC?
At the Wilderman Medical Clinic, we offer an interdisciplinary approach to addressing your pain, providing you with a personalized combination of treatments to best address your condition, including:
Interventional pain management for pudendal neuralgia:
• Nerve block injections for pudendal neuralgia
• Lidocaine infusion
• Ketamine infusion
Non-interventional pain management for osteoarthritis of the thoracic facet joints:
• Psychotherapy
• Kinesiology education sessions
Works Cited
Finnerup, N. B., Attal, N., Haroutounian, S., McNicol, E. D., Baron, R., Dworkin, R. H., Gilron, I., Haanpää, M., Hansson, P., Jensen, T. S., Kamerman, P. R., Lund, K., Moore, A. W., Raja, S. N., Rice, A. S., Rowbotham, M. C., Sena, E. S., Siddall, P. J., Smith, B. H., & Wallace, M. S. (2015). Pharmacotherapy for
neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurology, 14(2), 162–173. https://doi.org/10.1016/s1474-4422(14)70251-0
Grujičić, R., MD. (2022, December 22). Pudendal nerve. Kenhub. https://www.kenhub.com/en/library/anatomy/pudendal-nerve
Labat, J., Riant, T., Robert, R., Amarenco, G., Lefaucheur, J., & Rigaud, J. (2008). Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourology and Urodynamics, 27(4), 306–310. https://doi.org/10.1002/nau.20505
Leslie, S. W., Antolak, S., Feloney, M. P., & Soon-Sutton, T. L. (2022, November 28). Pudendal Neuralgia. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK562246/
Levesque, A., Bautrant, E., Quistrebert, V., Valancogne, G., Riant, T., Beer Gabel, M., Leroi, A.-M., Jottard, K., Bruyninx, L., Amarenco, G., Quintas, L., Picard, P., Vancaillie, T., Leveque, C., Mohy, F., Rioult, B., Ploteau, S., Labat, J.-J., Guinet-Lacoste, A., … Robert, R. (2022). Recommendations on the management of pudendal nerve entrapment syndrome: A formalised expert consensus. European Journal of Pain (London, England), 26(1), 7–17. https://doi.org/10.1002/ejp.1861
Wang, X., Wang, L., Li, Y., Lu, G., Zhao, G., & Feng, Z. (2022). Risk Factors and a Nomogram for Prediction of Refractory Pudendal Neuralgia: A Retrospective Multivariate Analysis Study. Pain Physician, 25(6), E815–E822.
Zhang, D., & Song, T. (2021). The Clinical Efficacy of High-Voltage Long-Duration Pulsed Radiofrequency Treatment in Pudendal Neuralgia: A Retrospective Study. Neuromodulation, 25(8), 1372–1377. https://doi.org/10.1111/ner.13401

