Covered by OHIP?
Most services are covered by the Ontario Health Insurance Plan (OHIP)
Waiting Time
Your timeframe depends on the type of procedure.
OHIP Covered Services
Most services are covered by the Ontario Health Insurance Plan (OHIP)
WILDERMAN MEDICAL CLINIC
Anatomy of the jaw
The word jaw describes the lower part of the face, starting from the inner corners of the eyes to the chin and reaching up to the bottom of the ears. It is composed of two separate parts: the upper and lower jaws.
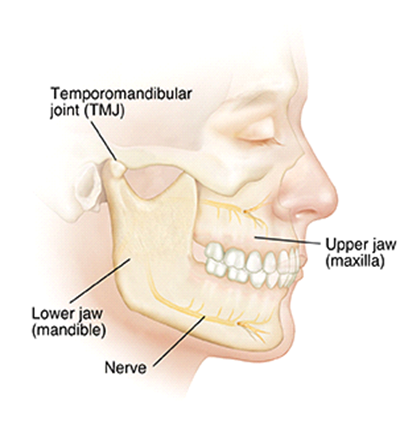
The upper jaw is attached to the skull and is called the maxilla. It starts at the inner corner of the eyes and descends to the lips. It forms part of the eye socket and the nasal cavity, and its lower end is where the upper teeth are attached.
The lower jaw is called the mandible and is the largest disconnected bone of the skull. It forms the cheeks and the chin as distinctive facial features. The lower teeth are attached to the upper portion. It is shaped like a horseshoe and stretches to the bottom of the ears.
Both of these parts are attached to the temporomandibular joints and are surrounded by muscles, nerves, and blood vessels. The primary purpose of the jaw is to crush food so the body can process it in the stomach and intestines.
It also plays a part in vocalizing (talking, singing, beatboxing, etc.).
What is jaw pain?
Jaw pain describes all painful sensory input that is felt in the jaw area. The causes of the jaw pain may originate from another body part but may be a helpful indicator of where the issue is. Jaw pain is a symptom, not a disorder in itself.
There are many possible causes for jaw pain, each with its own diagnosis criteria and treatments (Jaw Pain: Common Causes and How to Treat It, 2021). It is possible to have chronic jaw pain, and the intensity and/or type of pain can vary greatly between causes and individuals.
This article will introduce you to the most common causes of jaw pain, how these disorders are diagnosed, and how they are treated.
Note: If you are a woman/AFAB (assigned female at birth) suffering from sudden jaw pain with any of the new symptoms described below, please call 911 as you may be suffering from a heart attack:
- Uncomfortable pressure/fullness/squeezing/pain in the middle of your chest; this feeling may come and go
- Pain/discomfort through one or both arms, the neck, back, or stomach
- Feeling out of breath
- Cold sweats
- Nausea/vomiting
- Feeling light-headed or faint
- Exhaustion
- Dizziness/vertigo
Men/AMAB (assigned male at birth) may also experience jaw pain as a symptom of a heart attack, but it is less common.
Common causes of jaw pain
The symptom of jaw pain can be caused by many different disorders of varying degrees of severity.
The most common causes of jaw pain are:
- Bruxism: Also known as nightly teeth grinding, this disorder can lead to strained muscles, inflamed joints, broken teeth, and pinched nerves. It affects an estimated 10% of adults and 15% of children. The causes of bruxism include high stress/anxiety, smoking, excessive caffeine intake, and taking selective serotonin reuptake inhibitors (SSRI), which are a type of anti-anxiety medication. People with bruxism often feel jaw pain upon waking and may find that they aren’t sleeping well. Other symptoms include fractured teeth, sore jaw muscles, earaches, and headaches.
- Temporomandibular joint disorder (TMJ): TMJ is a disorder where one or both jaw joints are injured (Buescher, 2011). This injury causes pain and difficulty moving the jaw properly.TMJ can be caused by traumatic injuries, arthritis, night grinding, and some infections. Other symptoms of TMJ are earache, a popping/clicking sound when moving your jaw, a shift in the position of your lower jaw, and/or a new onset of headaches or migraines.TMJ affects an estimated 8% of people, with women/AFAB being four times more likely to be diagnosed with it than men/AMAB.
- Arthritis: Arthritis is a disorder that affects the joints throughout the body and may affect the temporomandibular joint. It causes the joints to become inflamed or start to break down. Jaw pain caused by arthritis may be accompanied by difficulty eating, drinking, or talking. Arthritis affects an estimated 20% of adults and 2% of children, but the jaw is rarely affected. It is more common in women/AFAB.
- Abscessed tooth: When a bacterial infection finds a hold in the mouth, a tooth abscess may form. This abscess is a pocket of pus, located by a tooth, that can spread if left untreated. It can cause jaw pain, often described as throbbing, which may be continuous or become sharp when chewing. It may radiate throughout your jaw, neck, or ear. Other symptoms include tooth sensitivity, bad breath, swelling of the jaw in the affected area, fever, or a red, swollen bump at the site of the abscess.
- Facial trauma: Facial trauma can easily cause jaw pain, whether temporarily until the injury heals or it can become chronic pain if the injury causes more permanent damage. The type of facial injury dictates what the treatment will be; treatments can range from icing the affected area, in the case of a bruised jaw, to reconstructive surgery for a major traumatic facial injury.
- Infections: There are many bacteria and viruses that can cause jaw pain. Infections may act on joints, muscles, nerves, or glands that can be found in the jaw. In the most serious of infections, the jaw may lock and prevent someone from being able to eat or drink.
Some infectious causes of jaw pain are:
- Sinusitis: A viral or bacterial infection of the sinus. The pressure from the congested sinus may extend into the jaw and cause pain.
- Mumps: A viral infection of the parotid glands, which makes saliva. It has no treatment except for managing the symptoms until it has run its course. The measles, mumps, and rubella vaccine has helped reduce its presence in the population.
- Tetanus: A bacterial infection that affects the nerves and causes muscles to lock. As it often impacts the neck and face, tetanus can cause lockjaw syndrome, which is accompanied by pain and an inability to open the mouth. The tetanus vaccine helps prevent the spread of the bacteria after a possible infection.
Your doctor or dentist may prescribe antiviral or antibacterial medication for the infection.
- Gum disease: Gingivitis is a common disease that causes the gums to become inflamed. This inflammation may lead to jaw pain, which can be worsened while eating or drinking. Periodontitis, which is a bacterial infection of the gums, may also cause jaw pain.
- Dental disorders: As your teeth are closely linked to your jaw, any issues related to them may lead to jaw pain. These disorders may include cavities, chipped/broken teeth, growing wisdom teeth, and/or exposed root nerves. The jaw pain caused by dental disorders is often sudden and recurring.
- Heart disorders: Jaw pain can be a symptom of a heart attack, one seen primarily in women/AFAB though some men/AMAB have reported feeling jaw pain during a heart attack. If the jaw pain appears without cause, is radiating, and is accompanied by a sign described above, then please contact your local emergency services (911).
Jaw pain can also be caused by heart arrhythmias, in which the heart has an irregular or dangerous beat.
- Cluster headaches: Cluster headaches are severe and acute headaches that start behind the eye. They happen several times a day, last less than four hours, and continue for weeks or months before stopping. This pain may radiate into the jaw and down the neck during an episode. The pain is debilitating and may be accompanied by nausea, restlessness, a swollen, teary, or red eye, and excessive sweating.
The exact cause of cluster headaches is unknown, but research has shown that it involves three systems: the trigeminovascular system, the parasympathetic system, and the hypothalamus (Del Mar Dominguez Garcia et al., 2023).
Cluster headaches affect around 0.1% of adults.
Diagnosis
As there are many causes of jaw pain, it is important that your doctor or dentist take your pain seriously and seek out the root cause of it (Krishna et al., 2010).
Here are some information and tests your doctor/dentist may use to find the cause of your jaw pain (De Leeuw & Klasser, 2018):
- Orofacial Pain Prospective Evaluation and Risk Assessment Questionnaire: This 20-question questionnaire can help identify TMJ based on risk factors and symptoms.
- Location, type, severity, and duration of your pain
- Risk factors such as smoking, excessive drinking, mental health issues, and past traumatic facial injuries
- Physical examination of your jaw: the presence of swelling, sores, bumps, or bruises may indicate certain causes
- 3-questions Erwin test for cluster headaches
- What helps and/or worsens your jaw pain
If your doctor/dentist believes it is necessary, they may send you for further testing. This may include an X-ray, an ultrasound, and/or blood tests.
Treatments
As there are many causes of jaw pain, the treatments for your pain will differ and be specific to the cause of your issue. Some treatment options are:
- Pain management medication
- Oral care
- Non-steroidal anti-inflammatory medication
- Antiviral and antibacterial medications
- Icing or heating the affected area
- Mouthguard
- Facial massage
- Botox injections
- PRP injections
- PRF injections
- Cortisone injections
- Prolotherapy
- Changing oral habits: this may include stopping smoking, drinking alcohol or soft drinks, increasing oral care, and addressing mental health disorders that may impact your oral health.
- Physiotherapy and exercises
If the jaw pain is severe, you may need surgery to address the root cause of your pain. This can range from a root canal to reconstructive surgery.
What do we do at WMC?
At the Wilderman Medical Clinic, we offer a variety of interventional and non-interventional treatment options aimed at reducing pain and increasing function.
These options include:
- Assessment and treatment of TMJ disorder
- Assessment and treatment of cluster headaches
- Assessment and treatment of bruxism
- Botox injections
- PRP injections
- PRF injections
- Prolotherapy
- Chronic pain counseling and prescription pharmaceuticals for pain management
- Genetic testing for customized medication prescription
Non-interventional pain management for osteoarthritis of the TMJ joint:
- Psychotherapy
- Kinesiology (exercises) education sessions
Works cited
Buescher, J. J. (2011). Temporomandibular Joint Disorders. American Family Physician. https://doi.org/10.1007/springerreference_44524
De Leeuw, R., & Klasser, G. D. (2018). Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management (By The American Academy of Orofacial Pain; 6th ed.). Quintessence Publishing.
Del Mar Dominguez Garcia, M., Abejón, D., De Diego Gamarra, J. M., Cánovas Martinez, M. L., Balboa Díaz, M., & Hadjigeorgiou, I. (2023). Symptoms and pathophysiology of cluster headache. Approach to combined occipital and supraorbital neurostimulation. Revista Española De Anestesiología Y Reanimación (English Edition), 70(1). https://doi.org/10.1016/j.redare.2021.10.005
Jaw Pain: Common Causes and How To Treat It. (2021). Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/24447-jaw-pain
Krishna, S., Badam, R., & Sobti, G. (2010). Diagnostic Perils in Jaw Pain. World Journal of Dentistry, 1(3), 187–192. https://doi.org/10.5005/jp-journals-10015-1037

