Covered by OHIP?
Most services are covered by the Ontario Health Insurance Plan (OHIP)
Waiting Time
Your timeframe depends on the type of procedure.
OHIP Covered Services
Most services are covered by the Ontario Health Insurance Plan (OHIP)
WILDERMAN MEDICAL CLINIC
About Post-Herpetic Neuralgia
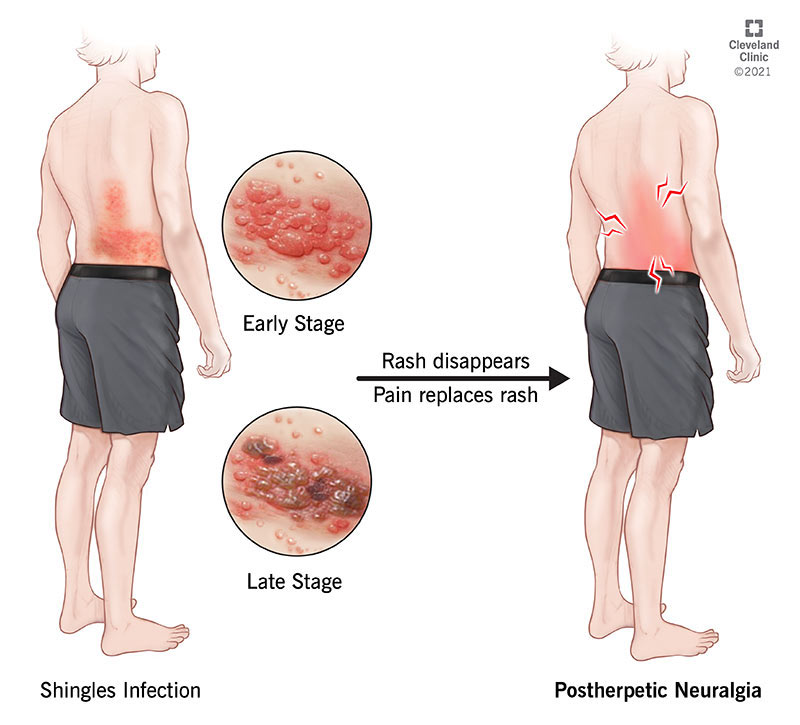
Post-herpetic neuralgia is pain that continues due to nerve damage that occurs when a patient suffers from shingles.
Post-herpetic neuralgia is typically pain that lasts for longer than three months after a shingles rash subsides.
Who is affected?
Approximately twenty percent of patients who have shingles will develop post-herpetic neuralgia.
Shingles are caused by the same virus that causes chickenpox, so anyone who has had chickenpox in their lifetime is susceptible to developing shingles, and potentially post-herpetic neuralgia. The risk of developing post-herpetic neuralgia increases with age and is greatest after the age of 60.
Having a compromised immune system also increases the risk of developing this condition.
What are the symptoms?
Typical symptoms of post-herpetic neuralgia include burning, aching, or throbbing pain at the site of the original shingles rash.
Sharp or stabbing pain may also occur at this site. Other sensations may include itching, numbness, or sensitivity to temperature or touch (allodynia). A patient may also suffer from headaches.
What causes it?
Shingles can occur when the virus that is responsible for chicken pox (herpes zoster) is reactivated in the body after lying dormant for years.
This results in a painful and blistering rash that can last for up to a month. During the shingles flare-up, the affected nerves may become damaged. This can result in an alteration in the signals that are sent from the nerves to the brain.
The resulting pain can be chronic and may last years after the shingles rash has cleared.
How is the condition diagnosed?
Your doctor will be able to diagnose this condition based on a medical history and the symptoms that you are experiencing. Medical tests are typically not required to diagnose post-herpetic neuralgia.
What are potential treatments?
Early intervention can be key for preventing post-herpetic neuralgia. At the first sign of shingles, seek medical attention.
If antiviral medication is given within three days of developing shingles, the risk of post-herpetic neuralgia is reduced by half.
The most commonly used medications to treat pain caused by post-herpetic neuralgia include anti-convulsant medications, serotonin-norepinephrine reuptake inhibitors, non-steroidal anti-inflammatory medications for mild cases, and opioids for more severe cases.
Numbing skin patches and topical creams are also available alternatives.
Mild doses of tricyclic antidepressants can also help reduce the perception of pain and improve sleep. In very serious cases, electrical nerve stimulation may also be an option for pain relief.
Patients should be well aware of the side effects that exist for the above-mentioned pain medications, some of which include psychological disturbances, addiction, swelling, weight gain, urinary retention, dizziness, and drowsiness.
A healthy diet, moderate exercise, regular sleep schedule, stress and depression-coping skills, and a positive attitude can also help to deal with the chronic pain caused by post-herpetic neuralgia.
Treatments we offer
Medications
We can prescribe medications to help treat your post-herpetic neuralgia pain.
Lidocaine infusion
Lidocaine is a local anesthetic. Intravenous (IV) lidocaine infusion can be used to treat post-herpetic neuralgia. Neuropathic pain, such as that related to post-herpetic neuralgia occurs when changes occur to pain receptors that allow more rapid activation of signaling pathways.
Lidocaine interferes with these signaling pathways and because of this has been used in treating various forms of neuropathic pain.
The adverse effects that are most common with this form of treatment include dizziness and confusion, tiredness, nausea and vomiting, changes in vision, and numbness. Patients are not allowed to drive for 24 hours after infusion.
We recommend they make travel arrangements for the day of infusion.
Nerve block injections
During nerve block injections for postherpetic neuralgia a numbing medication is injected into the affected nerves. This can result in significant and long-lasting pain relief (success varies significantly from patient to patient).
Botox injections
Botox is being increasingly used for the treatment of neuropathic pain, including post-herpetic neuralgia.
Injecting the affected area with Botox has been shown to significantly reduce pain for up to 16 weeks. The pain relief can take up to two weeks to take effect.
This treatment has also been associated with improvements in sleep.
This treatment is costly and we suggest patients check their coverage with their private insurance.
Ketamine IV
Ketamine is an anesthetic medication that relieves pain via multiple pathways.
Intravenous (IV) ketamine can also be used to treat the pain associated with post-herpetic neuralgia. This treatment has been associated with a rapid reduction (up to 50%) in pain caused by post-herpetic neuralgia.
Usually, treatment starts with four weekly or bi-weekly infusions – subject to be discussed with your attending physician. Patients are not allowed to drive for 24 hours after infusion.
We recommend they make travel arrangements for the day of infusion.

